In today’s rapidly evolving medical landscape, physicians are increasingly called upon to balance innovation with evidence, patient expectations with system constraints, and emerging tools with deeply rooted traditions. For Dr. Julie Chen — a leader in genomic precision medicine, board-certified in internal medicine, and fellowship-trained in integrative medicine — that means reclaiming what medicine was always meant to be: comprehensive, compassionate, and grounded in science.
“We all went into medicine to help people heal,” said Dr. Chen. “But many of us find ourselves navigating systems that are optimized for disease management, not for prevention. That isn’t a personal failing. It’s a systems problem.”
Dr. Chen currently serves as Chief Medical Officer at Radence, a company pioneering a multimodal precision-based model of care. At its core, Radence seeks to identify and intervene on disease risk earlier than traditional models allow — not in response to pathology, but in anticipation of it.
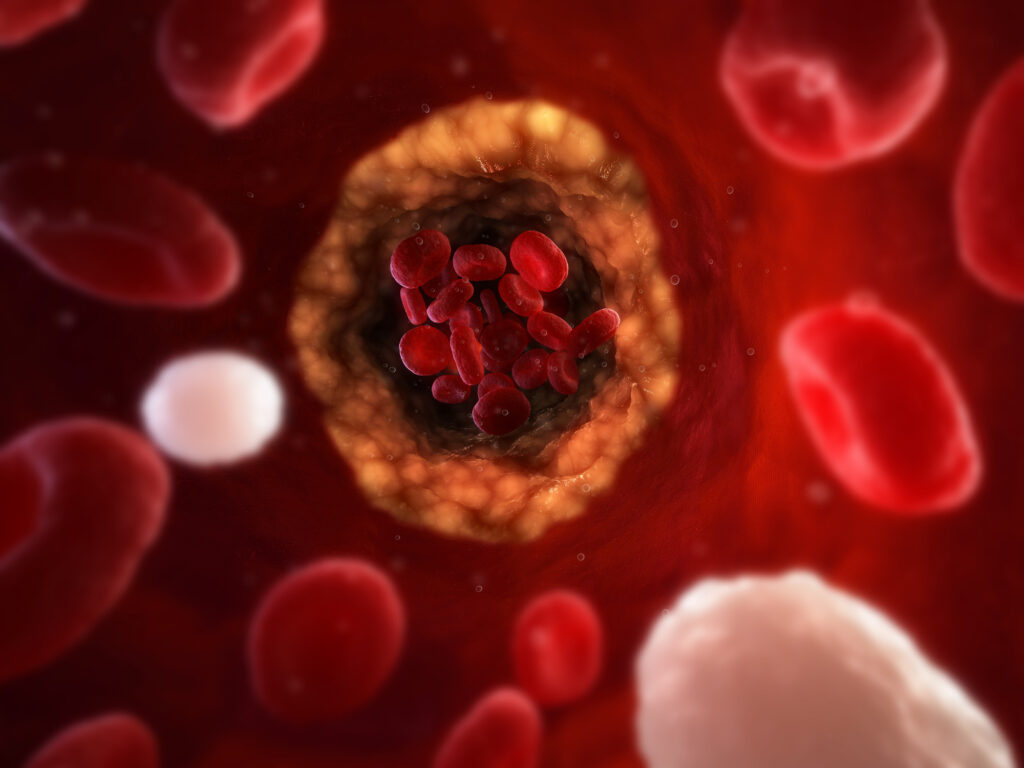
“Most of what we see in chronic disease is not sudden,” Dr. Chen said. “It’s a long, progressive breakdown of physiologic resilience. Our job is to understand that trajectory and to act on it early, when the patient still feels ‘fine,’ but the biology is already shifting.”
Addressing the Limits of Traditional Care
Dr. Chen has tremendous respect for the goals of current conventional medicine. However, she sees it as incomplete.
“Our traditional system is remarkable at acute intervention,” she said. “But it’s less equipped to manage early disease interception of the slow-developing dysfunctions that characterize so many of our biggest health challenges — cancer, cardiovascular disease, neurodegeneration, metabolic dysfunction.”
She points to constraints many physicians know well: 15-minute visits, fragmented specialty care, limited tools for subclinical disease, and a reactive rather than predictive infrastructure.
“It’s not that doctors don’t care about prevention or early detection,” Dr. Chen said. “It’s that the system doesn’t always give them the time or tools to do it well.”
A Multimodal, Systems-Oriented Approach
What Radence offers is a framework to augment what clinicians are already doing. Its platform brings together genomics, imaging, metabolomics, advanced blood work, and wearable data to generate a comprehensive picture of an individual’s health trajectory.
“We use high-resolution tools to pick up signals that traditional workups might miss. But more importantly, we translate those findings into real-world decisions. We help people understand their risk and take steps to modify it,” Dr. Chen said.
That process is deeply collaborative. Radence doesn’t seek to replace a patient’s care team. It works in partnership with referring clinicians, offering extended assessments and evidence-based recommendations that complement existing care plans.
“This is not about displacing primary care or specialists. It’s about supporting them with another layer of data and insight,” Dr. Chen said. “We know that no one understands the patient better than their own doctor. Our role is to enhance that relationship, not compete with it.”
Precision without Elitism
One concern often raised about precision or concierge medicine is equity—that these models only serve the affluent. Dr. Chen sees this differently.
“Early adopters always pave the way for broader access,” Dr. Chen said. “Every major medical advance — from medications to whole-genome sequencing — started in specialized settings before becoming standard. What we’re building now will eventually become more scalable. But someone has to lead, and that’s where Radence comes in.”
To that end, the company is investing in outcomes research, clinical validation, and real-world evidence to support its protocols. “We’re not just innovating,” she said. “We’re validating. We’re contributing to the science so this model can expand.”
Data Alone is Not Enough
Despite Radence’s technological sophistication, Dr. Chen emphasizes that data is only as powerful as the context it’s given.
“We’re not just handing people dashboards,” she said. “We’re walking them through it. We pair high-resolution diagnostics with meaningful conversation. That’s where trust is built. That’s how change happens.”
The result is more than early detection testing. It’s engagement.
“When patients understand their physiology, when they see the why behind a recommendation, they are more likely to act,” Dr. Chen said. “We’re not just changing lab values. We’re changing behavior.”
Four Disease Domains, One Coordinated Strategy
Radence begins by focusing on the survival layer — the four disease categories responsible for the majority of premature mortality and morbidity: cancer, cardiovascular disease, metabolic dysfunction, and neurodegeneration. These are not isolated silos, Dr. Chen noted. They are deeply interconnected through shared pathways of inflammation, oxidative stress, metabolic regulation, and genetic risk.
“If you have insulin resistance, you’re not just at risk for diabetes. You’re at increased risk for dementia and cardiovascular disease,” she said. “We take a systems-level view of risk. That means we can intervene in ways that impact multiple domains simultaneously.”
From there, the platform expands to assess autoimmune risks, hormone regulation, immune function, and more.
“We meet the patient where they are, and then we grow with them,” Dr. Chen said. “It’s dynamic. It’s continuous. And it’s deeply personal.”
An Invitation to the Medical Community
For Dr. Chen, one of the most innovative aspects of Radence is the partnership.
“We want to work with clinicians who are curious, collaborative, and committed to pushing the standard of care forward,” Dr. Chen said. “Whether you’re a cardiologist, internist, neurologist, or family physician, there’s a place for you in this model. We need your insight. Your experience. Your trust.”
She knows that change is never easy, especially in a field as high-stakes and evidence-driven as medicine. But she also knows that physicians are problem-solvers.
“We’re not asking people to abandon conventional care,” Dr. Chen said. “We’re inviting them to build on it. To extend it. To make it better.”
In an era where both patients and clinicians are demanding more — more answers, more support, more continuity, Dr. Chen sees Radence as a blueprint for what’s possible.
“This is the future of care: science-led, system-aware, patient-centered, and clinician-empowering,” Dr. Chen said. “We’re not starting over. We’re starting ahead.”